Overactive Bladder
What is an overactive bladder?
Overactive bladder, also called OAB, describes a combination of symptoms that can include:
-An uncontrolled frequent and sudden urge to urinate.
-Pass to urinate many times during the day and night.
-Urgency incontinence.
These symptoms can disrupt your life, even if you are able to get to the toilet in time when you feel an urge to urinate.
Symptoms
-The difficulty of controlling the sudden urge to urinate.
-Urgency incontinence.
-Urinate few times in 24 hours.
-Wake up few times at night to urinate.
Follow the link for more information about the symptoms of overactive bladder.
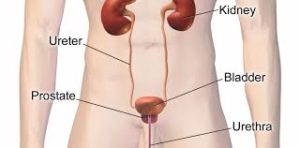
Causes
-Weak pelvic muscles: Pregnancy and childbirth can lead to the fragility of the pelvic muscles; so the bladder will sag out of its normal position. All of these factors can cause leakage.
-Nerve damage: Trauma and diseases (Parkinson’s, multiple sclerosis) can cause the damage of the nerves that sent signals to the brain and bladder to squeeze urine out of the body; so the patient will empty his bladder at the wrong time.
-Medicines that cause a rapid increase in urine production.
-Excess consumption of caffeine or alcohol.
-Infection: A urinary tract infection (UTI), can irritate the bladder nerves and cause compression to the bladder.
-Excess weight: The overweight causes extra pressure on your bladder. This can lead to urge incontinence.
-Hormonal deficiency in estrogen after menopause
Sometimes the doctor doesn’t find a cause for the overactive bladder.
Risk factors
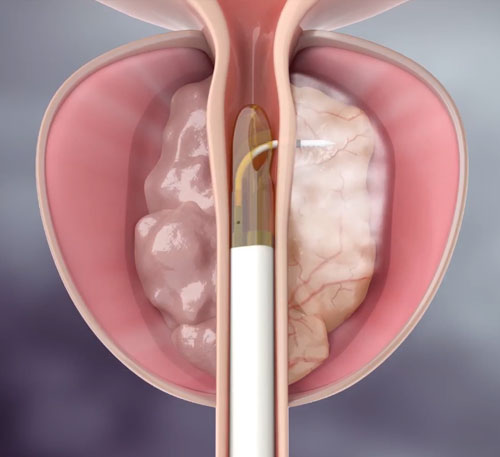
-Age: You have a high risk of having an overactive bladder when you get older. Age also raises your risk of other conditions that affect bladder control: BPH, diabetes…
-Women have more risk of developing an overactive bladder than men for several causes that affect the hormones and the pelvic muscles: menstruation, pregnancy, and menopause.
-Obesity
-People who have certain diseases like stroke or multiple sclerosis.
Complications
Overactive bladder can affect your life and cause:
-Depression.
-Anxiety.
-Sleep disorders (Waking up often at night to pee).
-Negative effects on sexuality.
Follow the link, to learn more about the diagnosis and treatment of overactive bladder.